Artificial Intelligence
Cognitive Behavioural Therapy
Chronic Pain Management
Introversion - Extraversion
Thinking - Feeling
Judging – Perceiving
Sensing – iNtution
Five Factor Model
Myers-Briggs Type Indicator
Natural Language Processing
Institutional Review Board
I.INTRODUCTION
In recent years, healthcare has undergone a transformative shift towards personalized medicine, a groundbreaking approach that goes far beyond the traditional one-size-fits-all model [1,2]. This evolving paradigm, often referred to as precision medicine, recognizes that each individual’s health is a complex interplay of various factors, and it tailors healthcare initiatives to the unique characteristics of each patient. Beyond genetic and medical data, personalized healthcare now considers a broad spectrum of elements for personalization, including sociological, psychological, behavioural, and environmental factors. This holistic approach seeks to provide not only more effective treatments but also proactive, preventative strategies that align with an individual’s lifestyle, preferences, and specific health needs. In this era of personalized healthcare, patients are increasingly seen as active participants in their own care, and healthcare providers strive to create a bespoke healthcare experience that optimizes both health outcomes and the overall well-being of the individual.
The incorporation of behavioural and personality considerations into healthcare practices has demonstrated its efficacy in improving patient outcomes [3]. One notable example is in the realm of addiction treatment. Healthcare providers have increasingly recognized the significance of tailoring interventions to individual personalities and behaviours when addressing substance use disorders [4,5]. For instance, a patient with a history of impulsive behaviour and sensation-seeking tendencies may benefit from cognitive-behavioural therapy techniques that focus on impulse control and risk assessment, while a patient with high levels of anxiety and avoidance tendencies may respond better to therapies that address underlying emotional triggers. By customizing treatment plans to align with the individual’s personality traits and behavioural patterns, addiction treatment programs have achieved higher rates of success in achieving and sustaining recovery, ultimately improving the lives of those affected by addiction.
Pain is a critical and ubiquitous element in the realm of healthcare which serves as a prominent symptom, a diagnostic clue, and a focus of therapeutic intervention [6]. It is a universal human experience that can manifest in various forms and durations. Chronic pain [7] is a persistent and enduring discomfort that can last for months or even years, profoundly affecting individuals’ daily lives. It often defies simple solutions and necessitates a comprehensive, multifaceted approach to management, as its causes can be complex and multifactorial. On the other hand, acute pain is characterized by its sudden onset and intense nature. It usually arises in response to specific triggers, such as injuries or illnesses, and serves as a crucial warning signal to the body. Acute pain tends to be shorter-lived compared to chronic pain and typically resolves as the underlying cause is treated or heals. Recognizing the differences between chronic and acute pain is vital not only for healthcare professionals but also for individuals experiencing pain. It informs the choice of appropriate treatments and interventions, aiming to alleviate suffering, restore functionality, and enhance overall well-being. Managing chronic pain involves a holistic approach to improve the individual’s overall well-being and function, while acute pain management primarily addresses the underlying issue causing the pain [8].
Chronic pain management (CPM) [9] is a critical aspect of healthcare that aims to alleviate or control pain, enhance patients’ quality of life, and improve their overall well-being. Traditionally, chronic pain management has been a uniform approach, with treatments and interventions prescribed based on the type and severity of pain. However, recent advances in artificial intelligence (AI) have paved the way for a more personalized and effective approach to pain management. Chronic pain can be debilitating and significantly impact a person’s quality of life, as it may limit their ability to perform daily activities, work, or engage in social and recreational activities. It can affect various parts of the body, such as the back, joints, muscles, nerves, or even be more generalized. Managing chronic pain can be challenging and often requires a multidisciplinary approach. Treatment options may include medication, physical therapy, psychological therapy, lifestyle modifications, and in some cases, surgical interventions. Additionally, alternative therapies like acupuncture, massage, and mindfulness techniques may also be beneficial in managing chronic pain. It’s crucial for individuals experiencing chronic pain to work closely with healthcare professionals to develop a comprehensive pain management plan tailored to their specific needs and circumstances.
Personality psychology has played a significant role in driving research interest in understanding the behavioural foundations of an individual. Personality, in essence, refers to the distinctive patterns of thinking, feeling, and behaving that arise from a combination of inherent temperaments, inclinations, and external factors such as environments and experiences [10]. Personality traits serve as tangible psychometric measures for explaining human behaviour. There are numerous personality traits that collectively make up an individual’s unique personality. These traits influence how people think, feel, and behave in various situations [11]. This paper explores the concept of personality-driven chronic pain management using AI, highlighting its potential benefits and providing examples of its practical application. It focuses on the intersection of personality psychology, AI, and pain management, highlighting how AI-driven personality assessment can lead to more tailored and effective approaches to pain relief. The relationship between personality and pain perception, expression, and management is a complex and multifaceted one. Various personality traits and factors can influence how individuals experience and cope with pain. We delve into the intricate relationship between personality traits and pain, illustrating key correlations. Neuroticism, extraversion, conscientiousness, agreeableness, openness to experience, resilience, sensitivity, empathy, and coping styles are key factors influencing pain perception, expression, and management. The following Table I lists few examples that highlight how understanding a patient’s personality can help healthcare providers tailor pain management strategies to their unique needs and preferences, ultimately leading to more effective and patient-centered care.
Table I. Examples of correlation of personality traits with pain management approaches
| Personality Trait | Sample Pain Management Approaches |
|---|---|
| Neuroticism and Pain Perception | Individuals with high levels of neuroticism tend to be more anxious and prone to negative emotions. This personality trait can amplify the perception of pain and make it more challenging to cope with. |
| Healthcare providers may need to incorporate anxiety-reducing techniques, such as mindfulness or relaxation exercises, into the pain management plan for such patients. | |
| Extraversion and Pain Coping | Extraverted individuals are often more sociable and outgoing. They may benefit from social support and distraction techniques when dealing with pain. |
| Incorporating group therapy or involving friends and family in the patient’s pain management can be particularly helpful for extraverted individuals. | |
| Conscientiousness and Adherence to Pain Medications | Conscientious individuals are typically organized and diligent. They may be more likely to adhere to a prescribed medication regimen and follow treatment plans precisely. |
| Healthcare providers can use this trait to their advantage by recommending structured medication schedules and setting clear expectations for treatment adherence. | |
| Agreeableness and Pain Communication | Patients with high levels of agreeableness may be more inclined to downplay their pain or avoid expressing their discomfort to avoid inconveniencing others. |
| Healthcare providers should encourage open and honest communication with these patients, ensuring that their pain is adequately assessed and addressed. | |
| Openness and Alternative Pain Management | Open-minded individuals may be more receptive to alternative or complementary pain management approaches, such as acupuncture, meditation, or herbal remedies. |
| Healthcare providers can discuss a range of options and collaborate with these patients to find therapies that align with their preferences. | |
| Resilience and Pain Coping Strategies | Resilience is the ability to bounce back from adversity. Patients with high resilience may benefit from pain management strategies that focus on building coping skills and psychological resilience. |
| This could include cognitive-behavioural therapy (CBT) to help them reframe their pain experiences positively. | |
| Introversion and Individualized Pain Management | Introverted individuals may prefer more individualized and self-directed pain management strategies. They might respond well to self-help resources, such as pain management apps or online support communities, where they can learn and manage their pain privately. |
| Sensory Sensitivity and Pain Threshold | Some personality traits can be associated with sensory sensitivity. For example, individuals with sensory processing sensitivity may have a lower pain threshold and may require more gentle or tailored pain management approaches to accommodate their heightened sensory experiences. |
Quite clearly, personality traits play a significant role in how individuals experience and cope with pain. Some people may be more resilient and adaptive, while others may have a lower pain tolerance and struggle with emotional aspects of pain. Recognizing these individual differences is crucial for tailoring pain management strategies effectively. At the same time, it’s important to note that personality is just one of many factors that influence pain perception and management. Pain is a complex phenomenon affected by biological, psychological, social, and cultural factors. Healthcare providers consider a patient’s personality traits alongside other factors when developing personalized pain management plans to ensure the most effective and holistic approach to pain relief.
The paper presents the Big Five personality trait theory [12] and the Myers-Briggs Type Indicator (MBTI) [13,14] as frameworks to understand how personality traits may impact chronic pain management. For each trait, we explore potential implications for pain perception and coping strategies. Furthermore, we introduce the concept of multimodal AI-driven personality assessment, which leverages data from various sources and modalities to create comprehensive personality profiles. These profiles provide deeper insights into an individual’s personality, which can inform personalized pain management plans. Ethical considerations are emphasized in data collection and analysis. Two illustrative case studies demonstrate the practical application of AI-driven personality insights in chronic pain management. These cases illustrate how understanding an individual’s personality traits can guide healthcare providers in crafting personalized pain management plans that align with the patient’s unique needs and preferences, resulting in improved quality of life and pain relief. The paper outlines the steps involved in creating a dataset for AI-driven personality assessment, emphasizing the collection of demographic information, medical history, pain-related data, psychological assessments, and treatment plans. It provides sample case studies illustrating how AI-driven personality assessment can inform personalized pain management plans for individuals with distinct personality profiles.
The paper marks the pioneering phase in the journey toward creation of an AI model tailored to deliver personalized chronic pain management recommendations grounded in an individual’s personality traits. The rest of the paper is organized as follows. Section II discusses some related work done in the field of personality-driven chronic pain management. In sections III and IV, the Big Five personality trait theory and the Myers-Briggs Type Indicator (MBTI) are presented as frameworks to understand how personality traits may impact chronic pain management. The concept of multimodal AI-driven personality assessment is introduced in section V. Section VI outlines the process of dataset creation, emphasizing the importance of selecting data sources, including patient records and psychological assessments, while considering privacy and ethical considerations, and lists potential data variables. Section VII provides illustrative case studies demonstrating the practical use of AI-driven personality insights in personalized pain management followed by highlighting the multifaceted potential impact of research on personalized pain management using AI-driven personality insights in section VIII. Finally, Section IX concludes the paper by summarizing the innovative AI-powered personalized pain management framework, acknowledging its potential and addressing key limitations in its implementation.
II.RELATED WORK
The pivotal work in the field of pain theory, originating with Melzack and Wall in 1965 [15], brought to the forefront the intricate interplay between psychosocial and physiological factors in pain modulation. This pioneering effort gave rise to the gate control theory of pain, a framework that comprehensively encompassed various elements influencing the perception of pain. Notably, it made a profound contribution to the scientific community by emphasizing the pivotal role played by both the central nervous system and psychosocial variables in shaping the experience of pain [16]. Subsequently, Melzack [17] extended the gate control theory of pain, merging it with stress models.
In numerous studies exploring the intricate relationship between personality and pain, there is a prevalent focus on personality disorders arising as a consequence of pain [18–22]. This focus underscores a fundamental aspect of research in this field, which is the recognition that prolonged and severe pain can have profound and far-reaching effects on an individual’s psychological well-being and personality structure. That is, the prevailing hypothesis in much of this research is that chronic pain serves as a catalyst for the development of personality disorders or the exacerbation of pre-existing personality traits. For example, individuals who were once characterized by resilience and emotional stability might find themselves becoming more neurotic or prone to mood disturbances due to the chronic pain’s relentless toll on their mental and emotional well-being. Conversely, those with pre-existing tendencies toward certain personality traits, such as high neuroticism or low extraversion, may find these traits accentuated under the ongoing stress of chronic pain.
Within the context of chronic pain, it becomes increasingly apparent that psychological factors carry a significant weight in determining an individual’s level of physical impairment, often surpassing the direct impact of the pain’s intensity. This observation underscores the intricate and multifaceted nature of chronic pain conditions, where the interplay between physical sensations and psychological responses plays a pivotal role in shaping a person’s overall experience. Chronic pain, by its very nature, is characterized by its persistence over an extended period, typically lasting for several months or even years. During this protracted ordeal, individuals often grapple with not only the physical discomfort but also a host of emotional and cognitive challenges. These psychological factors can include anxiety, depression, fear, frustration, and a sense of hopelessness, all of which can exacerbate the perception of pain and its impact on daily life. The profound influence of psychological factors on chronic pain can manifest in several ways such as pain perception, pain coping mechanisms, treatment outcomes and quality of life.
In a groundbreaking 2020 study by Ibrahim et al. [23], 102 individuals with persistent lower back pain, unresponsive to conventional treatments, underwent an extensive examination of the relationship between their personalities and pain experiences. Participants completed comprehensive personality surveys assessing temperament, fear of movement, anxiety, and sadness. Both males and females displayed lower “Openness to experience” and higher “Conscientiousness” scores compared to the general population. The study, after meticulous adjustments, revealed that neuroticism correlated with fear-avoidance, sadness, and anxiety. Conversely, extraversion and Openness to Experience were protective, associated with lower depression scores. Extraversion also inversely related to fear-avoidance, while Conscientiousness negatively correlated with sadness and anxiety.
In a 2022 parallel investigation by Hanney et al. [24], 124 individuals underwent personality assessments using the Eysenck Personality Inventory, focusing on neuroticism and extraversion. They also completed questionnaires about their pain experiences, revealing a significant connection between neuroticism and adverse pain-related outcomes. Those with higher neuroticism exhibited increased fear of movement, greater preoccupation with pain, heightened perception of its impact, and elevated pain severity. This study further categorized participants based on their personality profiles and pain experiences.
Despite the profound impact of psychological factors on chronic pain, it’s noteworthy that there remains a relative scarcity of conducted studies in this specific area. This research gap is a critical point to acknowledge because understanding the nuances of how psychological factors interact with chronic pain is vital for developing more effective treatment approaches. We illustrate this gap through a correlation diagram in Fig. 1.
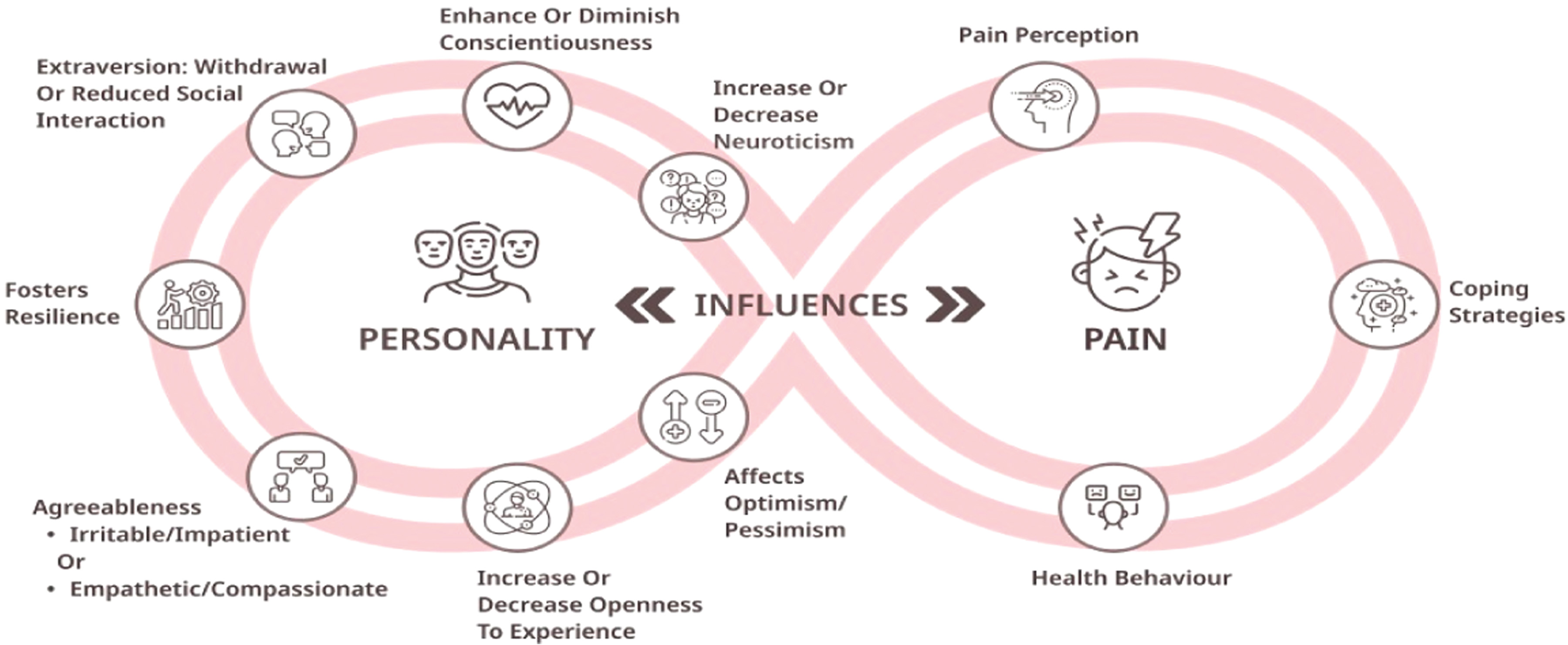 Fig. 1. Corelating pain and personality.
Fig. 1. Corelating pain and personality.
By conducting more comprehensive studies in this realm, researchers can gain deeper insights into the complex relationship between psychological factors and chronic pain. This knowledge, in turn, can lead to the development of targeted interventions that not only address the physical aspects of pain but also provide effective strategies for managing the psychological components, ultimately improving the overall well-being and functioning of individuals living with chronic pain.
III.BIG-5 PERSONALITY TRAIT THEORY AND CHRONIC PAIN MANAGEMENT
The Big Five personality traits [25], also known as the Five Factor Model (FFM), are a widely accepted framework in psychology that categorizes human personality into five broad dimensions (Fig. 2).
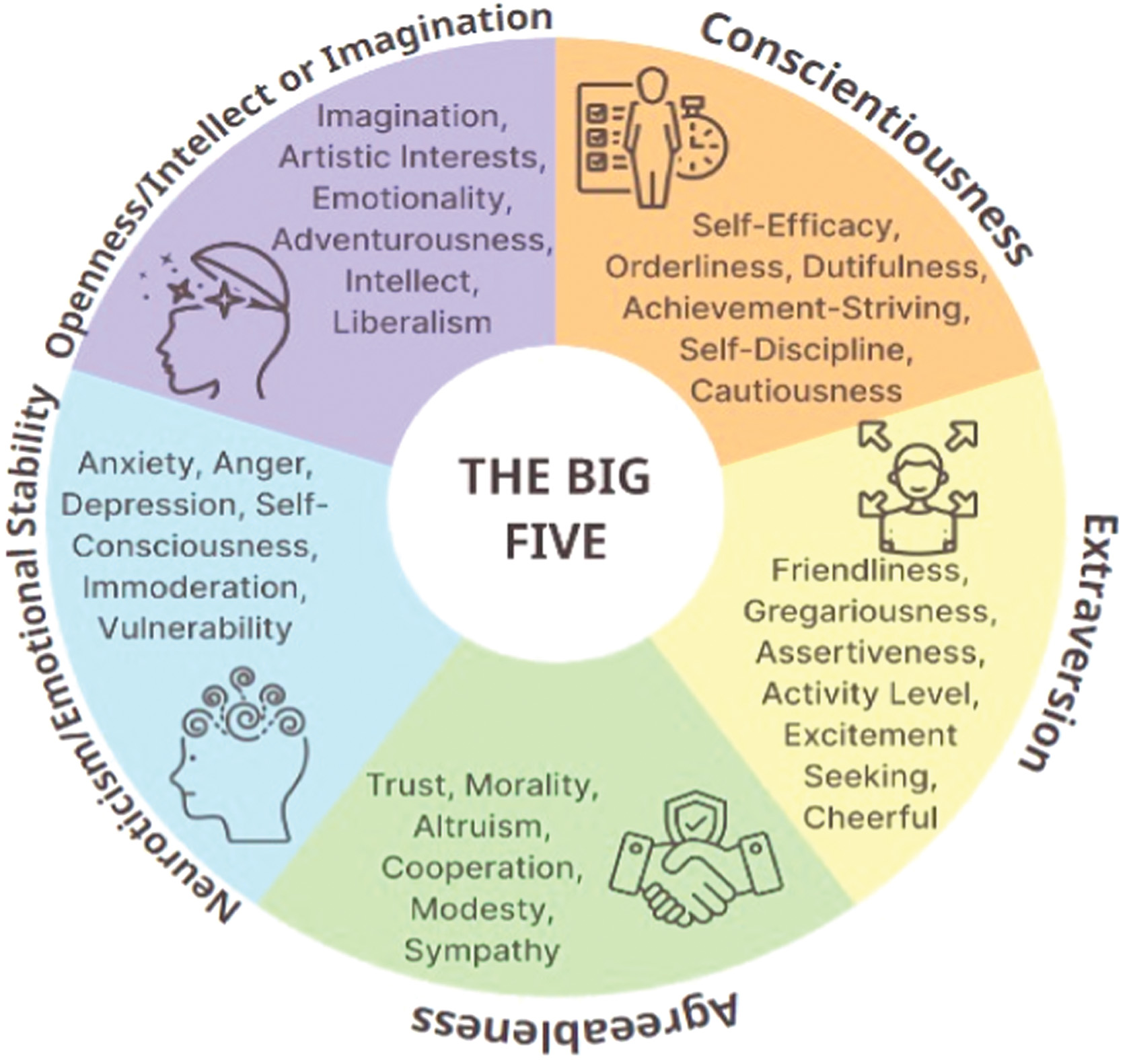 Fig. 2. Big-5 personality traits.
Fig. 2. Big-5 personality traits.
These traits are often used to understand and describe individual differences in personality. Here are the Big Five traits and their potential relevance to pain management:
- a.Openness to Experience: This trait reflects a person’s willingness to embrace new experiences, ideas, and intellectual curiosity. In pain management:
- •Patients with high openness may be more receptive to trying alternative or complementary pain management therapies, such as acupuncture, meditation, or unconventional treatments.
- •Healthcare providers can engage in open discussions with these patients, explaining various treatment options and encouraging them to explore new approaches.
- b.Conscientiousness: Conscientiousness relates to an individual’s level of organization, responsibility, and self-discipline. In pain management:
- •Highly conscientious patients may excel in following structured pain management plans, adhering to medication schedules, and keeping detailed records of their pain experiences.
- •Healthcare providers can provide clear, organized instructions and emphasize the importance of compliance with the treatment plan.
- c.Extraversion: Extraversion characterizes individuals who are outgoing, social, and energetic. In pain management:
- •Extraverted patients may benefit from social support as a coping mechanism for pain. Group therapy or involving friends and family in the patient’s pain management can be valuable.
- •Encouraging these patients to engage in physical activities and maintain an active lifestyle may also be effective.
- d.Agreeableness: This trait relates to an individual’s friendliness, cooperativeness, and concern for others. In pain management:
- •Agreeable patients may be more inclined to downplay their pain or discomfort to avoid burdening others. Healthcare providers should encourage open communication and reassure them that their well-being is a priority.
- •Collaborative decision-making and involving the patient in the treatment planning process can help address their agreeable nature.
- e.Neuroticism (Emotional Stability): Neuroticism reflects a person’s emotional stability and their tendency to experience negative emotions like anxiety, depression, and stress. In pain management:
- •Patients with high neuroticism may perceive pain as more intense due to heightened emotional reactions. Pain management for such individuals may focus on anxiety reduction and emotional regulation.
- •Techniques such as mindfulness, relaxation exercises, and cognitive-behavioural therapy (CBT) can be particularly useful.
Understanding a patient’s Big Five personality traits can help healthcare providers tailor pain management strategies to their unique characteristics and preferences. By considering these traits, healthcare professionals can provide more patient-centered care, leading to better pain management outcomes and improved patient satisfaction.
IV.MBTI PERSONALITY TRAIT THEORY AND CHRONIC PAIN MANAGEMENT
The Myers-Briggs Type Indicator (MBTI) is a widely used personality assessment tool based on the theories of Carl Jung [26]. It categorizes individuals into one of 16 personality types, each defined by a combination of four dichotomous preferences (Fig. 3).
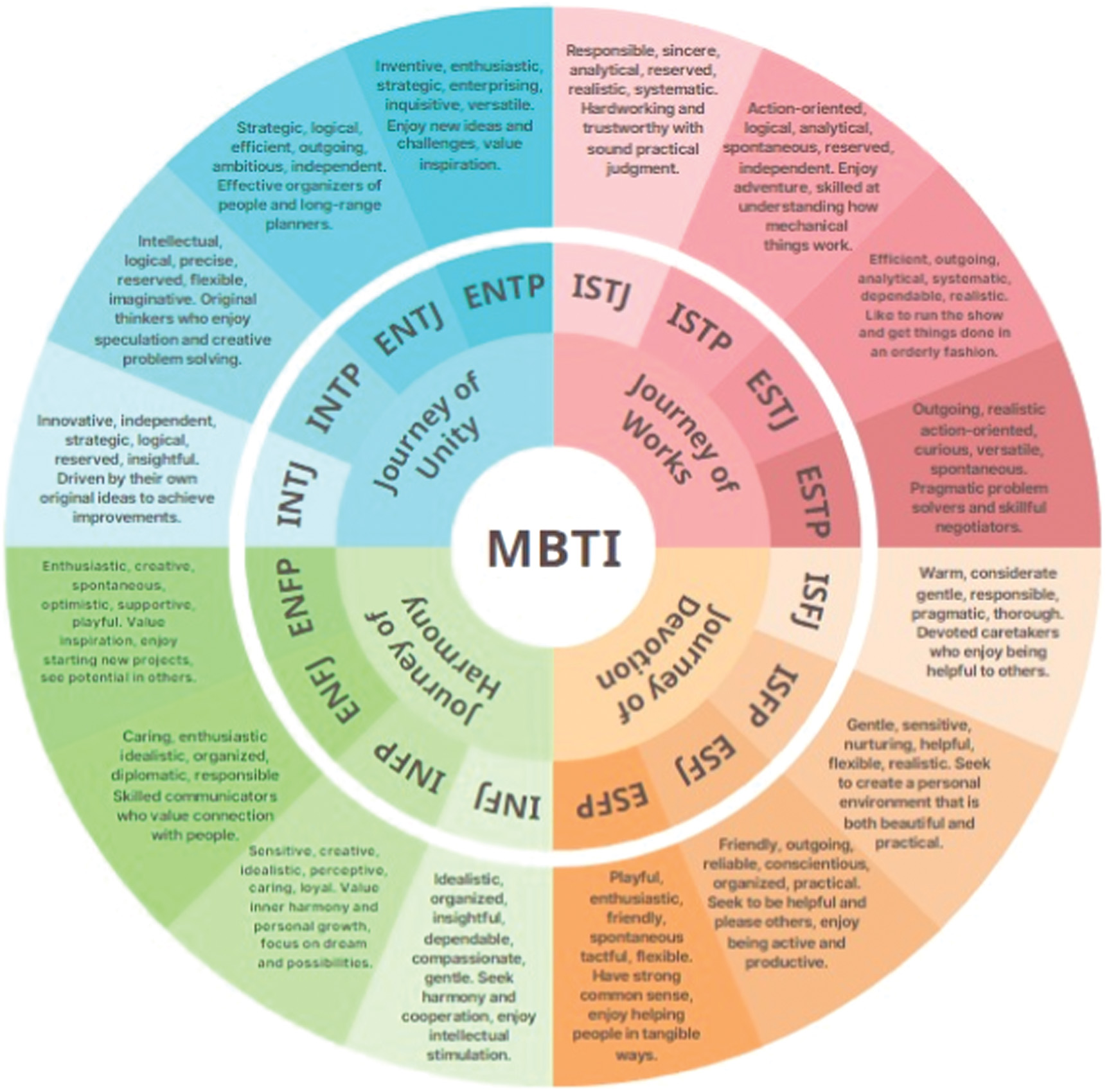 Fig. 3. MBTI personality traits.
Fig. 3. MBTI personality traits.
While MBTI is primarily used for understanding general personality traits and preferences, it can provide some insights into how individuals might approach pain management. Here’s how MBTI personality types might be related to pain management:
- a.Extraversion (E) vs. Introversion (I):
- •Extraverts (E) may seek social support and interaction as a coping mechanism for pain. Group therapy and involving friends and family in their pain management process could be beneficial.
- •Introverts (I) may prefer a more individualized approach to pain management, such as self-help resources, private reflection, or one-on-one therapy.
- b.Sensing (S) vs. Intuition (N):
- •Sensing types (S) tend to focus on concrete, practical details. They may prefer pain management strategies that are well-structured and based on proven, empirical methods.
- •Intuitive types (N) may be more open to unconventional or holistic pain management approaches that align with their creative and imaginative thinking.
- c.Thinking (T) vs. Feeling (F):
- •Thinking types (T) might approach pain management logically, relying on data and evidence-based treatments. They may be more comfortable discussing treatment options and potential risks.
- •Feeling types (F) may prioritize emotional well-being and may benefit from interventions that address the emotional aspects of pain, such as support groups and therapy focused on feelings and relationships.
- d.Judging (J) vs. Perceiving (P):
- •Judging types (J) tend to prefer structured and organized approaches to pain management. They may appreciate clear treatment plans, schedules, and specific goals.
- •Perceiving types (P) may be more flexible and adaptable in their pain management strategies, willing to try different methods and adjust their approach as needed.
It’s important to note that MBTI is a broad personality assessment tool, and personality traits and preferences are complex and multifaceted. People are not limited to the characteristics of their MBTI type, and individual experiences and responses to pain are influenced by various factors beyond personality.
V.MULTIMODAL AI-DRIVEN PERSONALITY ASSESSMENT
AI can analyse vast amounts of data, including patient records, psychological assessments, and even social media profiles, to create a comprehensive personality profile. This profile can encompass traits which can provide insights into how a patient may respond to pain and pain management interventions. Multimodal AI-driven personality assessment is an advanced approach that combines data and information from multiple sources and modalities to gain a more comprehensive understanding of an individual’s personality traits, preferences, and behaviour. These modalities can include text, speech, facial expressions, physiological signals, and more. This holistic approach allows for a richer and more accurate characterization of personality. Here’s an overview of multimodal AI-driven personality assessment as shown in Fig. 4.
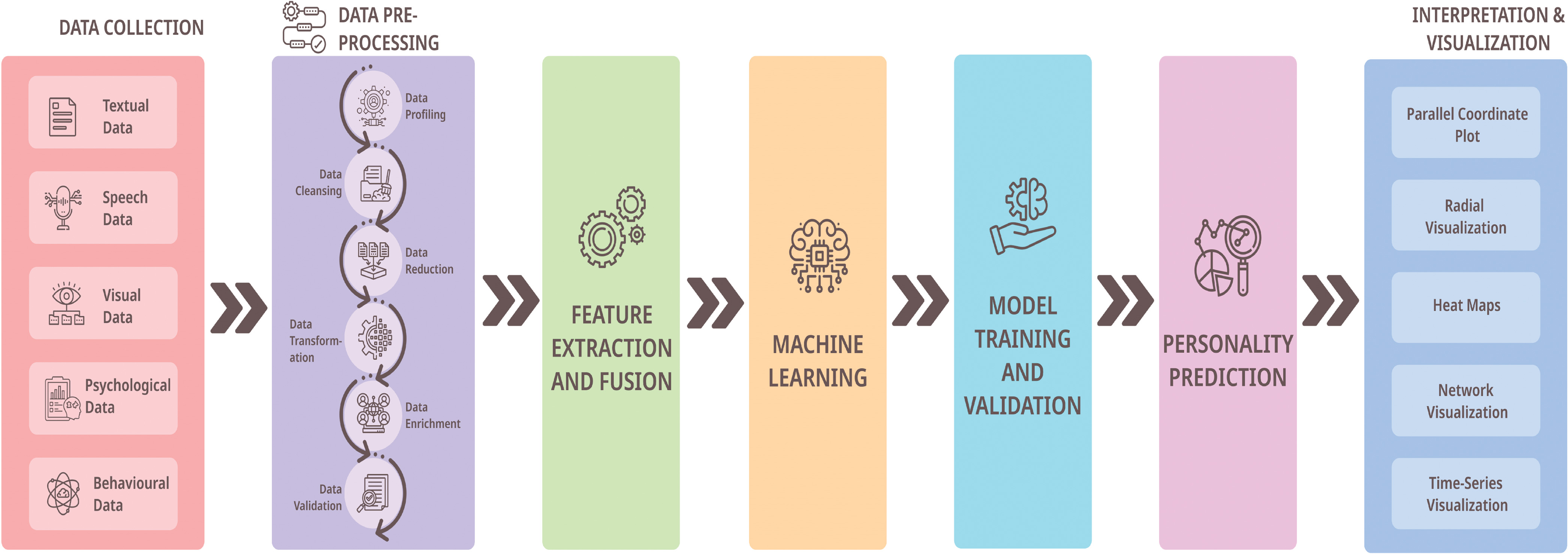 Fig. 4. Systematic diagram for multimodal AI-driven personality assessment.
Fig. 4. Systematic diagram for multimodal AI-driven personality assessment.
The following sub-sections discuss the details of the model.
A.DATA COLLECTION FROM MULTIPLE MODALITIES
Multimodal assessment begins by gathering data from diverse sources and modalities [27]. These sources encompass textual data, including social media posts, emails, and chat transcripts, which offer insights into written communication. Speech data, such as voice recordings, phone calls, and interviews, provide valuable auditory information. Visual data sources, such as facial expressions, body language, and eye movements, offer a visual perspective on behaviour. Physiological data, including heart rate, skin conductance, and brain activity, provide insights into the body’s responses [28,29]. Finally, behavioural data, encompassing online browsing habits, social interactions, and response times, offer a window into actions and interactions within digital environments. Further, mobile apps such as MyPain®1 can serve as the interface through which patients input their data. The app can create a secure user registration system, prioritize data input forms for patients to share personality traits, pain history, and preferences, and implement robust data validation checks to ensure accurate and complete user-submitted data. This comprehensive approach allows for a holistic understanding of an individual’s behaviour and personality traits.
B.PREPROCESSING FOR EACH MODALITY
In the preprocessing phase for each data modality, specific steps are taken to address the unique characteristics of the data type. For instance, text data typically undergoes natural language processing (NLP) techniques such as sentiment analysis, topic modelling, and linguistic feature extraction to extract meaningful insights from written content. Speech data is processed to recognize emotions, analyse pitch variations, and assess voice quality, enabling the extraction of emotional cues from spoken interactions. Visual data, on the other hand, is subjected to analyses that include facial expression recognition and the interpretation of body language, providing valuable information about non-verbal communication. Finally, physiological data is carefully filtered and synchronized to facilitate time-series analysis, allowing for a deeper understanding of physiological responses over time. These preprocessing steps are crucial in preparing the diverse data modalities for subsequent analysis and interpretation within the multimodal personality assessment framework.
C.FEATURE EXTRACTION AND FUSION
In the process of feature extraction and fusion, the goal is to capture pertinent information about an individual’s behaviour and personality from each data modality. This involves isolating and quantifying distinctive aspects of the data that can reveal insights about the person. Subsequently, features from various modalities can be integrated or fused together to form a comprehensive multimodal feature vector. This amalgamation of features from different sources creates a holistic representation of the individual, allowing for a more nuanced understanding of their behaviour and personality traits. The techniques employed for feature fusion can vary, including methods such as concatenation, stacking, or more advanced fusion strategies, selected based on the specific application and characteristics of the data under analysis. This stage plays a pivotal role in synthesizing information from diverse sources to create a more comprehensive profile of the individual’s personality and behaviour.
D.MACHINE LEARNING MODELS
In the context of multimodal personality assessment, machine learning models [30] come into play to harness the richness of the collected data. These models are trained using multimodal data to make predictions related to personality traits or behavioural characteristics of individuals. The selection of these models can vary, encompassing both traditional machine learning algorithms and more advanced deep learning architectures, specifically designed to handle the complexity of multimodal data. These models rely on labelled datasets where personality traits are either known through observation or self-reported by individuals. Through this training process, machine learning models become proficient at recognizing patterns and relationships within the data, enabling them to provide valuable insights into the personality traits and behavioural tendencies of the individuals under examination.
E.MODEL TRAINING AND VALIDATION
Model training and validation are pivotal stages in the development of machine learning models for multimodal personality assessment [31]. During training, these models are exposed to the labelled datasets, where known personality traits and behavioural characteristics serve as the ground truth. The models learn to recognize patterns and relationships within the multimodal data, enabling them to make predictions based on new, unseen data. Validation is a critical step to ensure the reliability and accuracy of the trained models. In this phase, appropriate evaluation metrics tailored to the complexities of multimodal data are employed. These metrics gauge how well the models perform in predicting personality traits from the combined data sources. Given the multifaceted nature of multimodal data, specialized evaluation metrics account for the nuances and interactions between different modalities. One advanced technique often utilized in this context is cross-modal validation. Here, the models are tested not only on the same type of data that they were trained on but also on different modalities. This cross-modal evaluation helps verify that the models can generalize their predictions across various data sources, making them more robust and versatile. The overall objective of model training and validation is to ensure that the machine learning models can accurately and consistently predict personality traits based on the amalgamation of data from different modalities. This process is integral to producing reliable insights into individuals’ behaviour and personality, enhancing the overall effectiveness of multimodal personality assessment systems.
F.PERSONALITY TRAIT PREDICTION
Upon successful training and validation, the multimodal AI model is primed to perform one of its core functions: predicting personality traits based on fresh multimodal input data. This predictive capability represents a critical step in the application of multimodal personality assessment. When confronted with new input data, the model applies its learned knowledge and intricate understanding of the relationships within the data to make predictions regarding the individual’s personality traits. These predictions can be presented in various forms, typically tailored to the requirements of the specific personality assessment framework being employed. In some instances, the predictions are furnished as numerical scores, quantifying the likelihood or intensity of particular personality traits. These scores offer a nuanced view of an individual’s personality profile, highlighting the degrees to which specific traits are present. Such numerical scores can be valuable for researchers and practitioners seeking detailed insights into personality dynamics. Alternatively, the predictions can be expressed as categorical labels, assigning individuals to distinct personality types or categories. This approach is particularly beneficial when personality assessments follow categorical frameworks, such as the Myers-Briggs Type Indicator (MBTI), which classifies individuals into one of several personality types based on their traits. Ultimately, the multimodal AI model’s ability to predict personality traits from diverse data sources provides a powerful tool for understanding and characterizing individuals’ behaviour and personalities. These predictions contribute to personalized recommendations and interventions, enhancing the utility of personality assessment in various domains, including healthcare, education, and human resources.
G.INTERPRETATION AND VISUALIZATION
Interpretation and Visualization in multimodal personality assessment are crucial steps in making sense of the data and presenting it in a meaningful way. Interpretation involves the process of assigning significance and context to the personality traits that have been predicted. It aims to explain how these traits may influence an individual’s behaviour, decisions, and interactions. For instance, if the assessment indicates that an individual scores high in extraversion, the interpretation would delve into the implications of this, such as their tendency to be outgoing, sociable, and energized by social interactions. This contextualization helps stakeholders understand how personality traits manifest in real-world scenarios. Visualization techniques play a pivotal role in making the assessment results accessible and understandable. Personality trait radar charts are a common tool used for this purpose. In these charts, each personality trait is represented as a point on the radar chart, with the distance from the center indicating the intensity or score of that trait. This visual representation allows for quick and easy comparisons of an individual’s personality traits, giving a clear overview of their personality profile. Heatmaps are another valuable visualization method. They provide a visual summary of the relationships and correlations between different personality traits. By examining patterns in these heatmaps, analysts and researchers can gain insights into how specific traits interact with and influence one another, offering a deeper understanding of an individual’s personality dynamics. Interactive dashboards take the visualization a step further by providing a dynamic platform for exploring an individual’s personality profile. Users can interact with the data, zooming in on specific traits, timeframes, or other aspects of the assessment. This interactivity allows for a more in-depth exploration and analysis of an individual’s personality characteristics.
Overall, the interpretation and visualization of multimodal personality assessment results serve to bridge the gap between complex data and practical insights. They empower practitioners, researchers, and individuals themselves to make informed decisions, tailor interventions, and gain a clearer understanding of personality traits in various applications, including psychology, healthcare, and education.-
H.ETHICAL CONSIDERATIONS
Ethical considerations in multimodal personality assessment are of utmost importance [32,33], and they encompass several critical facets.
- •Informed Consent: Obtaining informed consent from individuals whose data is being collected is a fundamental ethical principle. Participants must be fully informed about the purpose of data collection, how their data will be used, and any potential risks or consequences. They should have the autonomy to decide whether they want to participate or not, without any form of coercion.
- •Data Privacy: Protecting the privacy of individuals is a central ethical concern. Personal data, especially sensitive data like physiological signals or facial expressions, should be handled with the utmost care. This includes secure storage, encryption, and strict access controls to prevent unauthorized use or breaches.
- •Anonymization: Whenever possible, data should be anonymized to remove any personally identifiable information. This helps mitigate the risk of data being traced back to specific individuals. Anonymization techniques must be rigorously applied to protect participants’ identities.
- •Transparency: Transparency in the assessment process is crucial. Participants should be informed about the algorithms and methods used for personality assessment. They have a right to know how their data is being analysed and how the results will be used.
- •Data Retention: Ethical considerations also extend to how long data is retained. Data should only be stored for as long as necessary for the intended purpose. Afterward, it should be securely deleted to minimize any potential risks associated with data breaches or misuse.
- •Bias and Fairness: Researchers and practitioners must be vigilant about addressing bias in data collection and analysis. Bias can arise from various sources, including the data itself or the algorithms used. Efforts should be made to identify and mitigate bias to ensure fair and equitable assessments.
- •Beneficence and Non-Maleficence: The ethical principles of beneficence (doing good) and non-maleficence (avoiding harm) should guide all actions in personality assessment. The assessment process should aim to benefit individuals while minimizing any potential harm or distress caused by data collection or interpretation.
- •Regulatory Compliance: Adherence to relevant data protection and privacy regulations is essential. Researchers and organizations must comply with local and international laws governing data collection, storage, and processing.
- •Ethical Review: In some cases, especially in research involving human subjects, an ethical review by an institutional review board (IRB) or ethics committee may be necessary. This external review ensures that the research aligns with ethical standards and safeguards the well-being and rights of participants.
- •Continuous Monitoring: Ethical considerations are not a one-time affair. Continuous monitoring and auditing of data handling practices should be in place to ensure ongoing compliance with ethical principles.
In summary, ethical considerations in multimodal personality assessment are multifaceted and require careful planning and execution. They are essential to protect the rights, privacy, and well-being of individuals involved in the assessment process and to maintain trust in the field of personality assessment.
Based on the personality assessment, AI can recommend personalized pain management strategies. Here are some examples:
- •Cognitive-Behavioural Therapy (CBT) [34]: For a patient with high neuroticism, AI may suggest CBT techniques that focus on managing anxiety and stress, which can exacerbate pain perception.
- •Pharmacological Interventions [35]: AI can recommend medication options, dosages, and schedules that align with a patient’s personality traits. For instance, individuals with high extraversion may respond better to medications that offer rapid relief, while those with high conscientiousness may prefer a structured and organized medication regimen.
- •Lifestyle Modifications: Patients with specific personality traits may benefit from lifestyle changes, such as mindfulness practices for individuals with high neuroticism or exercise routines for those with high extraversion.
- •Support and Education: AI can provide personalized educational materials and support resources tailored to the patient’s personality, helping them better understand and cope with their pain.
VI.BUILDING A DATASET FOR AI-DRIVEN PERSONALITY ASSESSMENT IN PAIN MANAGEMENT
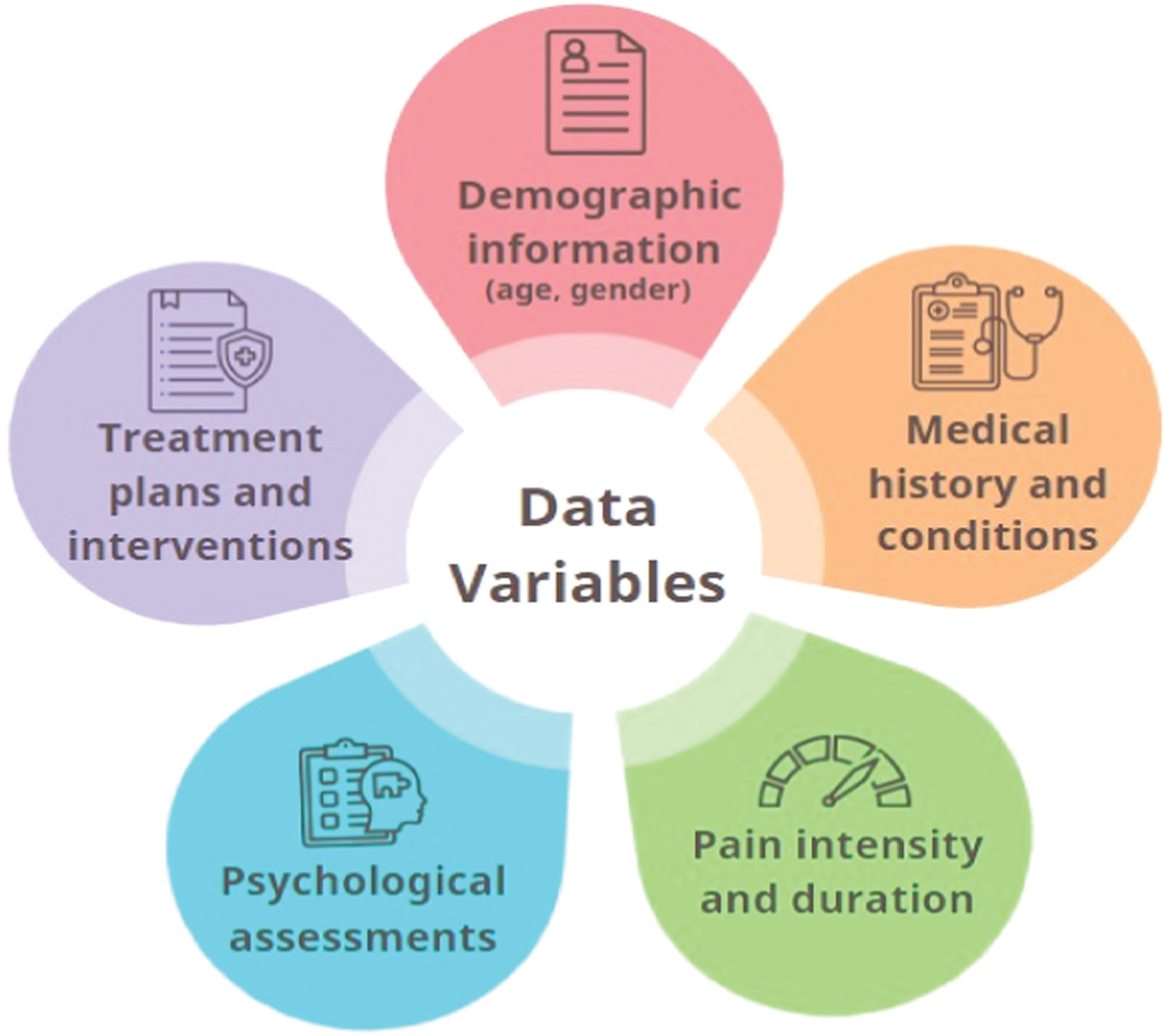
The objective of dataset creation is to gather data to assess personality traits and their relevance to pain management. Primarily, the sources of data used in creating the dataset, such as patient records, medical interviews, and psychological assessments should be finalized. Simultaneously considering anonymization for privacy and ethical considerations. A variety of data variables which can be collected include (but not limited to): demographic information (age, gender), medical history and conditions, pain intensity and duration, psychological assessments (e.g., Big Five personality traits), treatment plans and interventions as depicted pictorially in Fig. 5.
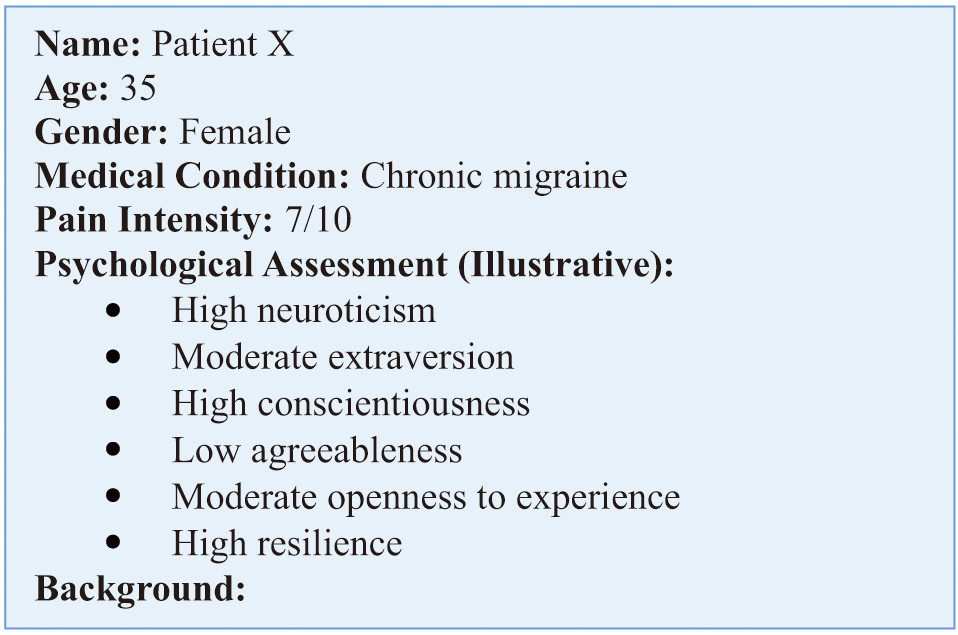
Figure 6 depicts an illustrative patient profile that serves as a foundational basis for crafting a personalized pain management plan, tailored to Patient X’s unique personality traits and needs. Such a plan would aim to alleviate her chronic migraine pain, enhance her overall well-being, and improve her quality of life.
VII.ILLUSTRATIVE CASE STUDIES FOR THE APPLICATION OF AI-DRIVEN PERSONALITY INSIGHTS IN THE CONTEXT OF PERSONALIZED PAIN MANAGEMENT
In this section of the paper, we present two detailed case studies referring to the subjects Maria and Anthony, illustrating the practical implementation of AI-driven personality insights in the context of personalized pain management. (Note: Names and identifying details have been altered to safeguard privacy and confidentiality). These case studies follow a structured format, encompassing the following key elements:
- •Patient Introduction: Each case study commences with an introduction to the patient, offering essential demographic information such as age, gender, and their underlying medical condition. In Maria’s case, her chronic lower back pain due to a herniated disc is highlighted, while Anthony’s story revolves around his battle with fibromyalgia, a chronic pain disorder.
- •AI-Driven Personality Assessment: The section provides a comprehensive overview of the AI-driven personality assessment process employed for each patient. This involves a thorough analysis of diverse data sources, including textual data extracted from medical records, information garnered from interviews and questionnaires, and multimodal data encompassing voice recordings from therapy sessions and facial expressions captured during consultations.
- •Personality Insights: For both case studies, we delve into the personality traits identified through the AI-driven assessment. These traits encompass neuroticism, extraversion, conscientiousness, agreeableness, openness to experience, and resilience. The interpretation of these traits within the context of each individual patient offers profound insights into their emotional dispositions, social inclinations, and potential coping mechanisms.
- •Personalized Pain Management Plan: The heart of each case study revolves around the development of a personalized pain management plan. The section delineates how specific aspects of the patient’s personality traits are harnessed to inform and tailor the treatment approach. For instance, Maria’s elevated neuroticism prompts the inclusion of anxiety reduction strategies, while Anthony’s pronounced extraversion emphasizes the importance of social engagement in his plan.
- •Progress and Outcome: Each case study concludes by summarizing the progress and outcomes achieved through the personalized pain management plans. This critical component underscores the practical benefits of integrating individual personality attributes into pain management strategies. Both Maria and Anthony demonstrate noteworthy improvements in pain management, coupled with enhanced emotional well-being, exemplifying the tangible advantages of this tailored approach.
A.CASE STUDY ONE
We present an example case study demonstrating personalized pain management using AI and personality insights.
“Meet Maria: A 32-year-old battling chronic lower back pain with the power of personalized pain management and AI-driven personality insights”
Patient’s Name: Maria
Age: 30
Gender: Female
Medical Condition: Chronic lower back pain due to a herniated disc
Personality Traits: High neuroticism, moderate extraversion, high conscientiousness, moderate agreeableness, moderate openness to experience, high resilience
Background:
Maria has been suffering from chronic lower back pain for several years. She has tried various treatments and therapies, but her pain persists, affecting her daily life and emotional well-being. Maria’s healthcare provider decides to implement a personalized pain management plan based on AI-driven personality insights.
AI-Driven Personality Assessment:
Using AI, Maria’s healthcare provider conducts a comprehensive personality assessment by analysing various data modalities, including text data from her medical records, interviews, and questionnaires, as well as speech data from her therapy sessions and facial expressions captured during consultations.
Personality Insights: Based on the AI-driven personality assessment, the following personality traits are identified:
- •High Neuroticism: Maria tends to experience heightened anxiety and negative emotions, which may contribute to her perception of pain.
- •Moderate Extraversion: She is moderately outgoing and open to social interactions, which could be leveraged for social support.
- •High Conscientiousness: Maria is highly organized and diligent, indicating a strong potential for adherence to a structured pain management plan.
- •Moderate Agreeableness: She is moderately cooperative and compassionate, but may downplay her pain to avoid inconveniencing others.
- •Moderate Openness to Experience: Maria is open to trying new experiences and therapies beyond conventional medicine.
- •High Resilience: Her ability to bounce back from adversity suggests a potential for effective coping strategies.
Personalized Pain Management Plan:
- •Neuroticism and Anxiety Reduction: Knowing that Maria has high neuroticism, her pain management plan includes regular sessions with a pain psychologist trained in cognitive-behavioural therapy (CBT). CBT techniques are tailored to address her anxiety and emotional distress related to pain.
- •Extraversion and Social Support: Maria 's moderate extraversion is leveraged by introducing her to a support group for individuals with chronic pain. Group therapy sessions provide a platform for her to share her experiences and receive emotional support from peers.
- •Conscientiousness and Structured Plan: Given her high conscientiousness, the pain management plan emphasizes a structured approach. Maria receives a detailed schedule for physical therapy sessions, medication reminders, and journaling exercises to track her pain experiences.
- •Agreeableness and Communication: To encourage open communication, Maria’s healthcare provider emphasizes that her pain is a legitimate concern. Maria is encouraged to report her pain accurately, enabling the provider to make necessary adjustments to her treatment plan.
- •Openness to Experience and Complementary Therapies: Maria’s willingness to explore new experiences aligns with her interest in alternative pain management approaches. Her plan includes options like acupuncture and mindfulness meditation in addition to traditional treatments.
- •Resilience and Coping Skills: Maria’s high resilience suggests her potential for developing effective coping skills. She is introduced to a pain coping skills workshop to help her reframe her pain experiences positively.
Progress and Outcome:
Over the course of several months, Maria’s personalized pain management plan yields positive results. Her pain becomes more manageable, and her emotional distress significantly decreases. She actively engages in group therapy, adheres to her treatment plan, and explores complementary therapies with an open mind. Maria’s improved pain management enhances her overall quality of life, allowing her to regain some of the activities she once enjoyed.
B.CASE STUDY TWO
Let’s look at another example case study demonstrating personalized pain management using AI and personality insights.
“Charting a New Course for Pain Relief: Anthony’s Story of Fibromyalgia and AI-Powered Personalized Care.”
Patient’s Name: Anthony
Age: 42
Gender: Male
Medical Condition: Fibromyalgia, a chronic pain disorder
Personality Traits: Low neuroticism, high extraversion, moderate conscientiousness, high agreeableness, moderate openness to experience, low resilience
Background:
Anthony has been living with fibromyalgia for several years, causing widespread pain, fatigue, and emotional distress. Traditional pain management approaches have had limited success in improving his quality of life. Anthony’s healthcare provider decides to employ AI-driven personality insights to create a personalized pain management plan.
AI-Driven Personality Assessment:
Anthony’s healthcare provider conducts an AI-driven personality assessment by analysing a variety of data sources, including text data from medical records, voice data from therapy sessions, and behavioural data from patient interactions.
Personality Insights: Based on the AI-driven personality assessment, the following personality traits are identified:
- •Low Neuroticism: Anthony experiences relatively low levels of anxiety and negative emotions.
- •High Extraversion: He is highly sociable, outgoing, and optimistic, seeking social interactions to boost his mood.
- •Moderate Conscientiousness: Anthony displays moderate levels of organization and responsibility, showing potential for adherence to a structured pain management plan.
- •High Agreeableness: He is highly cooperative, compassionate, and empathetic, which may impact how he communicates pain.
- •Moderate Openness to Experience: Anthony is open to trying new experiences and therapies beyond traditional medical approaches.
- •Low Resilience: His low resilience indicates that he may struggle with adapting to the emotional and psychological aspects of chronic pain.
Personalized Pain Management Plan:
- •Low Neuroticism and Emotion Regulation: Given Anthony’s low neuroticism, his pain management plan includes mindfulness-based stress reduction techniques and relaxation exercises to help him manage occasional pain-related anxiety.
- •High Extraversion and Social Engagement: His high extraversion suggests a preference for social interactions. Anthony is encouraged to participate in group therapy sessions where he can share experiences with others living with fibromyalgia.
- •Moderate Conscientiousness and Structured Routine: Anthony receives a structured daily routine, including exercise, medication schedules, and dietary recommendations. This approach aligns with his moderate conscientiousness.
- •High Agreeableness and Communication: Healthcare providers emphasize open and honest communication, as Anthony may tend to underreport his pain due to his high agreeableness. He’s assured that his well-being is a priority.
- •Moderate Openness to Experience and Holistic Therapies: Anthony’s willingness to explore new experiences is utilized by introducing complementary therapies like acupuncture, dietary supplements, and guided imagery alongside conventional treatments.
- •Low Resilience and Coping Skills: Recognizing his low resilience, Anthony is referred to a cognitive-behavioural therapy (CBT) program designed to help him build coping skills and resilience in the face of chronic pain.
Progress and Outcome:
Over time, Anthony’s personalized pain management plan yields positive results. He engages actively in group therapy, follows his structured routine, and embraces complementary therapies. While he may still experience pain, his improved coping skills and social support network help alleviate emotional distress, resulting in an overall enhanced quality of life.
These case studies exemplify the application of AI-driven personality insights in tailoring a pain management plan for an individual. By understanding Maria’s or Anthony’s unique personality traits, healthcare providers will be able to offer a more personalized and effective approach to her chronic lower back pain and fibromyalgia respectively, ultimately leading to improved well-being and pain relief.
VIII.POTENTIAL RESEARCH IMPACT
The research on personalized pain management using AI-driven personality insights has the potential to significantly benefit a broad spectrum of stakeholders in the healthcare ecosystem. Patients grappling with chronic pain conditions stand to gain by receiving tailored treatment plans that align with their unique personality traits, leading to improved pain relief, enhanced overall well-being, and reduced emotional distress. Healthcare providers can offer more effective, patient-centered care, resulting in higher patient satisfaction and better outcomes. Health institutions and insurance companies may see reduced healthcare costs due to fewer hospitalizations and unnecessary medical procedures. Researchers and academia can explore new dimensions in healthcare by integrating personality psychology with treatment strategies. Ethical committees and regulatory bodies can use the research to inform ethical guidelines for AI applications in healthcare, while health tech and AI developers can leverage it to create innovative tools. Ultimately, personalized pain management benefits not only individuals with chronic pain but also healthcare providers, institutions, insurers, researchers, and the broader healthcare community.
The research outlined in the paper, which focuses on personalized pain management through AI-driven personality insights, holds substantial potential for substantial impact across various domains.
- •Improved Patient Outcomes: One of the primary impacts is the potential to improve patient outcomes. By tailoring pain management plans to individuals’ unique personality traits, healthcare providers can enhance the effectiveness of treatment, reduce pain intensity, and improve overall well-being. This can lead to better quality of life for individuals suffering from chronic pain conditions.
- •Enhanced Patient-Centered Care: Personalized pain management recognizes patients as active participants in their care. It fosters a patient-centered approach where treatment plans are customized to align with patients’ needs, preferences, and personality traits. This approach can lead to higher patient satisfaction and engagement in their healthcare.
- •Reduced Healthcare Costs: Effective pain management can potentially reduce healthcare costs associated with chronic pain conditions. By tailoring treatments to individuals, unnecessary interventions can be avoided, and patients may experience fewer hospitalizations or emergency room visits.
- •Advancements in AI and Healthcare Integration: The research demonstrates the practical application of AI in healthcare, showcasing how AI-driven personality assessments can inform treatment plans. This could stimulate further advancements in AI technologies for healthcare, improving diagnostics, treatment recommendations, and patient monitoring.
- •Ethical Considerations: The research emphasizes ethical considerations in data collection and analysis. It highlights the importance of data privacy, informed consent, and transparency in using personal data for healthcare purposes. This can contribute to the development of ethical guidelines for AI applications in healthcare.
- •Research in Pain Management: The paper contributes to the evolving field of pain management by integrating personality psychology with treatment strategies. This interdisciplinary approach can inspire further research into the relationship between personality traits and pain perception, paving the way for more effective pain management techniques.
- •Patient Education: The research emphasizes the importance of patient education and support. Patients gain a better understanding of their pain and how it relates to their personality traits. This knowledge empowers them to take a more active role in managing their pain and making informed decisions about their treatment.
- •Holistic Approach to Pain Management: The research promotes a holistic approach to pain management, considering not only physical symptoms but also psychological and social aspects of pain. This broader perspective can influence how healthcare providers approach pain management in various contexts.
- •Improved Quality of Life: Ultimately, the impact of personalized pain management is reflected in the improved quality of life for individuals living with chronic pain conditions. By reducing pain and enhancing overall well-being, patients can lead more fulfilling lives, engage in daily activities, and participate in social and recreational activities they may have previously avoided.
It’s important to note that while the research demonstrates significant potential, further studies and real-world implementation are needed to validate its effectiveness across a broader range of chronic pain conditions and patient populations. Additionally, ongoing research and advancements in AI and healthcare technologies will continue to shape the impact of personalized pain management in the coming years.
IX.CONCLUSION
In conclusion, this paper introduces a groundbreaking and forward-thinking theoretical framework that merges the power of artificial intelligence (AI) with insights from personality psychology to revolutionize personalized chronic pain management. It delves deep into the intricate relationship between personality traits and how individuals perceive, express, and manage pain, uncovering significant correlations that shape the pain experience. This innovative approach, which combines established personality theories like the Big Five and the Myers-Briggs Type Indicator (MBTI) with cutting-edge multimodal AI-driven personality assessment, promises to usher in a new era of tailored pain management. Furthermore, the paper underscores the ethical considerations and the importance of meticulous data collection processes when implementing such AI-driven solutions in clinical practice. By presenting real-world case studies, it vividly illustrates how this framework can lead to more effective, patient-centered pain relief, ultimately enhancing overall well-being.
In essence, this paper advocates for the establishment of an “AI-Powered Holistic Pain Management Initiative.” Such an initiative has the potential to transform the landscape of chronic pain management by offering data-driven, personalized solutions. Its ripple effects extend beyond individual patient care, encompassing broader impacts on clinical practice, patient outcomes, healthcare policy, and our collective understanding of personalized medicine and AI-driven interventions. This holistic approach holds the promise of improving the lives of countless individuals living with chronic pain, marking a significant step forward in the quest for more effective and compassionate healthcare.
Despite the promising potential of the theoretical framework introduced in this paper for personalized chronic pain management, it’s essential to acknowledge and address several limitations in its implementation. First and foremost, concerns related to data privacy and security loom large, given the sensitive nature of the patient data involved. Safeguards and ethical protocols must be rigorously upheld to protect individuals’ information from misuse or breaches. Additionally, the success of AI-driven personality assessments relies heavily on the availability and quality of data, which can vary significantly in practice. The generalizability of findings is another critical consideration, as cultural, socioeconomic, and individual differences can influence how personality traits interact with pain experiences. Chronic pain itself is a complex phenomenon influenced by numerous factors beyond personality, and oversimplifying this intricate relationship can lead to incomplete assessments. Furthermore, the current capabilities of AI in understanding human personality pose potential accuracy and bias challenges that require ongoing development and refinement. Ethical guidelines, clear consent procedures, and considerations of autonomy must be established to ensure responsible AI use in healthcare. Lastly, the long-term effectiveness, sustainability, and patient acceptance of AI-driven interventions must be rigorously studied and validated to realize the full potential of this framework in improving personalized pain management.